WHAT IS PATELLOFEMORAL PAIN SYNDROME?
Patellofemoral pain syndrome (PFPS), often referred to as ‘runners knee,’ is a condition that results in pain in or around the kneecap. PFPS can affect runners and non-runners alike, commonly seen in the general population. In fact, it is one of the most common diagnoses seen in patients with knee pain from an unknown cause, with a reported prevalence as high as 22.7% in the general population.1
According to the Journal of Orthopedic and Sports Physical Therapy: PFPS is classified by pain experienced around the kneecap, particularly during squatting, ascending/descending stairs, or anytime the knee is flexed and loaded at the same time. Pain might also be elicited following a period of prolonged sitting.2
WHAT CAUSES PATELLOFEMORAL PAIN SYNDROME?
Many contributing factors can lead to PFPS, indicating a need for a skilled and nuanced evaluation to be performed by your PT or Primary Care Provider. Listed below are some of the common contributing factors to PFPS:
Above the knee joint
-
Hip adductors/internal rotators that overpower extensors/abductors/external rotators
-
Weak glutes, weak core, tight hip internal rotators
-
Individuals’ anatomic structure, tibiofemoral joint rotation (q-angle)
At the knee joint
-
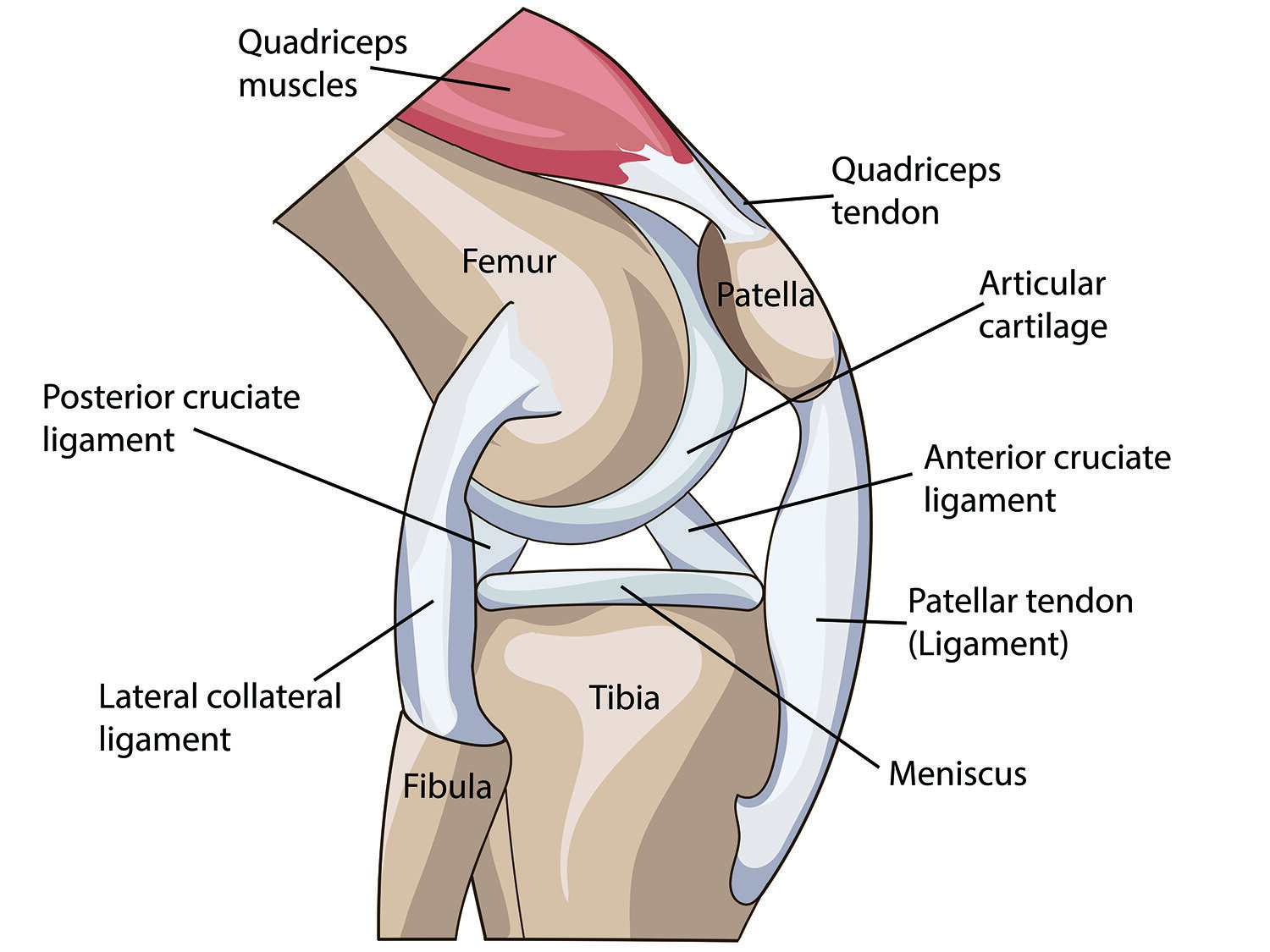
Lateral tracking of the patella caused by the medial motion of the hip joint
-
Patellofemoral or tibiofemoral joint capsule impairments
-
Knee ligament or quadricep tendon restriction
Below the knee joint
-
Ankle joint mobility and muscle imbalances
-
Altered landing pattern or running kinematics
-
Externally rotated foot during relaxed stance
-
Rearfoot eversion/pronation at heel strike
HOW CAN I TELL IF I HAVE PATELLOFEMORAL PAIN SYNDROME?
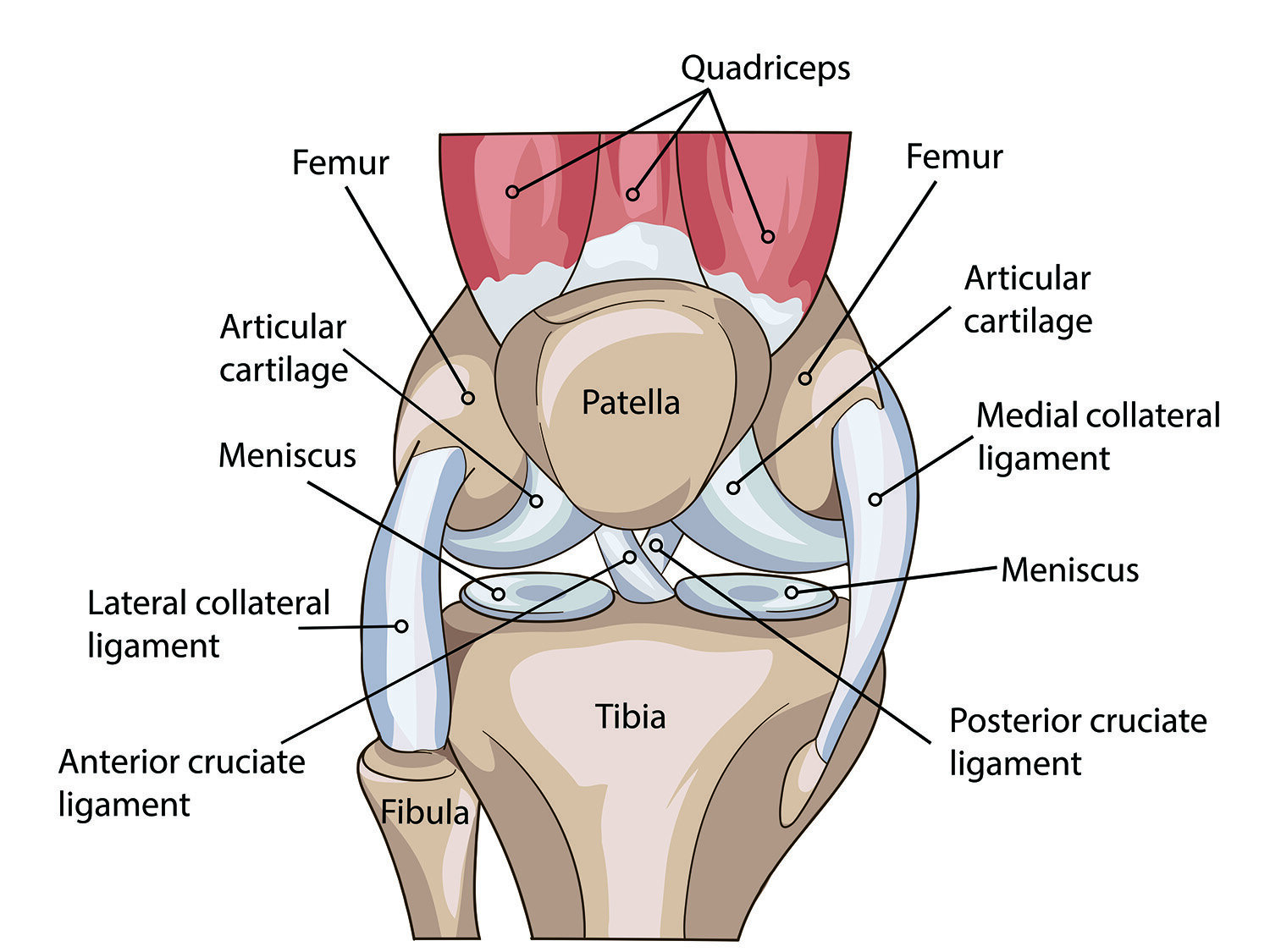
Many signs and symptoms can point you toward a diagnosis of PFPS. For example, pain “behind” or around the knee cap region, swelling or locking of the knee, feeling of the knee collapsing inward with activity, pain while ascending or descending stairs or squatting, and/or pain while landing after a jump. Additionally, if you experience decreased flexibility or muscle tightness of the hamstrings, quads, calves, or hips, you may be experiencing PFPS.
While these signs and symptoms can be helpful in understanding PFPS, it is important to be evaluated by a healthcare professional to receive an accurate diagnosis.
RUNNERS CORNER
Clinical experience shows us that runners who up their mileage rapidly tend to experience PFPS at higher rates. Furthermore, those with lower cadence, old training shoes, and concrete-heavy training appear to suffer PFPS more frequently. Physical therapy can help assess gait mechanics and running movement patterns that may lead to PFPS to avoid injury re-occurrence. In the acute stage, initial treatments often include specific stretching and strengthening routines and modifying training volume temporarily to reduce knee joint stress.
HOW CAN PHYSICAL THERAPY HELP?
Physical Therapy can be an effective tool to manage PFPS and create a specific routine that works for you. Some PT treatments for PFPS may include:
-
Hip targeted strengthening: with a focus on gluteus medius strength to prevent dynamic knee valgus collapse. Supine bridging for posterolateral hip control, and hip extension/abduction strength.
-
Gait and movement retraining to improve the dynamic alignment of your knees, so that you can better perform activities, including squatting, kneeling, walking, running, jumping, and climbing stairs
-
Knee targeted strengthening including squats and lunges for quadriceps strength, and single leg squats for postural control and retraining functional movement patterns.
-
Stretches, including kneeling hip flexor stretches to improve soft tissue mobility.
-
Manual therapies include myofascial release and joint mobilizations for improving range of motion and pain management.
-
Neuromuscular re-education of optimal movement patterns while running, squatting, or lifting, to decrease pain and prevent the risk of re-injury.
-
Therapeutic taping and bracing (McConnell, Kinesio tape) to decrease pain with activities.
-
Footwear and orthoses to support the improved alignment of your knees and lower extremities during daily activities and sport-related movement
Evidence has shown that a multi-modal approach drawing upon different treatment modalities has superior outcomes and improved return to play without reinjury.
AUTHOR:
Devin Wulff PT, DPT, CSCS
LWPT Kirkland Physical Therapist
CONTRIBUTORS:
Dr. Ghislaine Robert, MD
Sport & Spine Physician
Dr. Bob Adams, DO
Ret. USA Track & Field Head Medical Doctor, Sports Medicine Physician
Katie Hutchins, PT, DPT
Ben Wobker, PT, MSPT, CSCS, CFSC, SFMA
Founder & Director Lake Washington Physical Therapy
WHAT DOES THE RESEARCH SAY?
A combination of different treatment modalities is most effective for PFPS, including therapeutic exercises, manual therapy, and neuromuscular re-education. In one randomized controlled trial from 2021, Scafoglieri et al. found that manual therapy combined with local exercise in patients with a diagnosis of patellofemoral pain syndrome (PFPS) helped with pain reduction, force production, and functionality, more than the traditional local exercise therapy program.3 To further this point, a systematic review from 2015 concluded that therapeutic exercise was effective in reducing knee pain in patients with PFPS, with hip and knee exercises being more effective than knee exercises alone at reducing pain.4 Ultimately, a nuanced treatment approach tailored to the individual will provide the greatest pain relief and functional outcomes for each patient, with a combination of manual therapy, therapeutic exercises, and complementary modalities.
REFERENCES
-
Smith, B. E., Selfe, J., Thacker, D., Hendrick, P., Bateman, M., Moffatt, F., Rathleff, M. S., Smith, T. O., & Logan, P. (2017). Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS ONE, 13(1).
-
Willy RW, Hoglund LT, Barton CJ, Bolgla LA, Scalzitti DA, Logerstedt DS, Lynch AD, Snyder-Mackler L, McDonough CM. Patellofemoral Pain. J Orthop Sports Phys Ther. 2019 Sep;49(9):CPG1-CPG95. doi: 10.2519/jospt.2019.0302.
-
Scafoglieri A, van den Broeck J, Willems S, et al. Effectiveness of local exercise therapy versus spinal manual therapy in patients with patellofemoral pain syndrome: medium term follow-up results of a randomized controlled trial. BMC Musculoskelet Disord. 2021;22(1). doi:10.1186/s12891-021-04310-9
-
van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma‐Zeinstra SMA, van Middelkoop M. Exercise for treating patellofemoral pain syndrome. Cochrane Database of Systematic Reviews 2015, Issue 1. Art. No.: CD010387. DOI: 10.1002/14651858.CD010387.pub2. Accessed 09 August 2021.




